| Medical Aid in Dying (MAiD) Legalization Dates by State | |
| State | Legalization Date |
|---|---|
| Washington | 3/5/2009 |
| Montana | 12/31/2009 |
| Vermont | 5/20/2013 |
| California | 6/9/2016 |
| Colorado | 12/16/2016 |
| Washington, D.C. | 2/18/2017 |
| Hawaii | 1/1/2019 |
| New Jersey | 8/1/2019 |
| Maine | 9/19/2019 |
| New Mexico | 6/20/2021 |
Perspectives on Medical Aid in Dying: A Multifaceted Ethical Discussion
Featured Article
Ethics and Medical Aid in Dying: Physicians’ Perspectives on Disclosure, Presence, and Eligibility. DeCamp, Matthew, Julie Ressalam, Hillary D. Lum, Elizabeth R. Kessler, Dragana Bolcic-Jankovic, Vinay Kini, and Eric G. Campbell. 2023. Journal of Law, Medicine & Ethics 51 (3): 641–50. DOI: 10.1017/jme.2023.1001
Introduction
On February 2nd, 2024, the multi-institutional Society of Cutaneous Oncology (SoCO) Journal Club (JC) discussed the article titled “Ethics and Medical Aid in Dying: Physicians’ Perspectives on Disclosure, Presence, and Eligibility” published in Journal of Law, Medicine & Ethics. Participants included clinicians and researchers from Massachusetts General Hospital, Mass Eye and Ear, Brigham and Women’s Hospital, Dana-Farber Cancer Institute, George Washington Cancer Center, the National Institutes of Health, Columbia University Medical Center, University of Washington, Northwestern Medicine, Maine Health and the University of Sydney. The ensuing dialogue provided a diverse range of insights and opinions on the ethical complexities surrounding Medical Aid in Dying (MAiD). This Perspectives on the Science piece reflects the collective viewpoints of the authors post-discussion, distinct from the perspectives of other Journal Club members or their affiliated institutions. Here, we present an overview of the discussion focused on this contribution to the field.
Background
Overview and Evolution of Medical Aid in Dying
Medical Aid in Dying (MAiD), also known as physician-assisted death, is a practice that allows terminally ill or incurable patients to end their lives by taking prescription of lethal medications prescribed by a physician. Developments in MAiD over the years reflect medical advances, changing societal attitudes, and evolving ethical and legal frameworks.
Current Legalization Status
Between 2009 and 2021, ten US States or jurisdictions legalized MAiD, reflecting a growing acceptance of the practice (Table 1).2–8 The geographical spread of MAiD legalization across the country provides a clear illustration of its growing acceptance and the diverse legal interpretations it engenders.
States Considering MAiD Legislation and Specific Cases
Thanks to legislative efforts nationwide, several other states are actively considering laws related to MAiD (Figure 1).
The Massachusetts Medical Aid in Dying Bills (H.2246 and S.1331), which are currently under consideration, were reviewed as an example of how MAiD legislation is crafted with consideration of ethical, medical, and legal concerns. The bills outlines eligibility criteria, emphasizing mental capacity and terminal illness prognosis, and mandates a process that includes multiple patient requests, physician assessments, and a waiting period(Tables 2-3). Massachusetts House and Senate Medical Aid in Dying Bills provide comprehensive details.9,10
Comparative Analysis of MAiD Regimens
Originally characterized by the use of drugs like secobarbital and pentobarbital, MAiD now includes various drug regimens, such as DDMP, DDMP2, DDMA, and DDMAPh (Tables 4-6), each designed to ensure a peaceful and dignified end-of-life experience.These regimens demonstrate reflect the specialized nature of MAiD, with using lethal dosages that are significantly higher than typical therapeutic use dose ranges.11 In many cases anti-nausea/pro-gastric motility drugs are provided before drinking the MAiD suspension.12
It is important to note that data on the utility and side effects of specific regimens are limited, and there is a lack of consensus in the medical community regarding the optimal approaches for MAiD.12 Recent studies and reviews highlight this the evidence gap.13 They point to the need for further research into the pharmacokinetics and pharmacodynamics of these drugs at the high dosages used in MAiD. In the absence of objective evidence, practitioners and policymakers must rely on multidisciplinary expert opinions that incorporate clinical expertise, ethical considerations, and patient preferences.
Bridging the Gap: From MAiD’s Background to Ethical Considerations in Practice
Despite technical advances, legalizations, and growing societal acceptance of MAiD, there remain unmet needs in understanding and addressing the ethical complexities of this practice. The featured study, “Ethics and Medical Aid in Dying: Physicians’ Perspectives on Disclosure, Presence, and Eligibility” by DeCamp et al., aims to address this gap.1 By exploring physicians’ perspectives, this study sheds light on the ethical considerations that healthcare providers must navigate in the context of MAiD and end-of-life care.
Study Design
The study, conducted in Colorado, surveyed physicians likely involved in MAiD-related activities. Using a previously described sampling strategy,14 researchers identified physicians providing outpatient care to patients similar to actual MAiD patients. Surveys were distributed by mail.
Main Findings
The study revealed diverse opinions among physicians on MAiD. Key findings include varied attitudes towards disclosure of personal views on MAiD to patients, willingness to be present during MAiD drug ingestion, opinions on expanding MAiD eligibility, and the perceived utility of ethics consultations.
Discussion
These findings underscore the complexity of MAiD as a medical practice. They reflect a spectrum of ethical considerations, personal beliefs, and professional responsibilities that healthcare providers must navigate in the context of MAiD. During the February 2nd session, we conducted an informal survey to better understand the experience of members of the SoCO Journal Club. A subset of the questions in our survey were adapted from those used in the Colorado study. While a direct comparison is not feasible due to differences in survey design and population, this approach does provide an opportunity for contextual comparison, offering insights into the perspectives of SoCO Journal Club members in relation to those of the physicians surveyed in Colorado.
Professional Roles and Perspectives
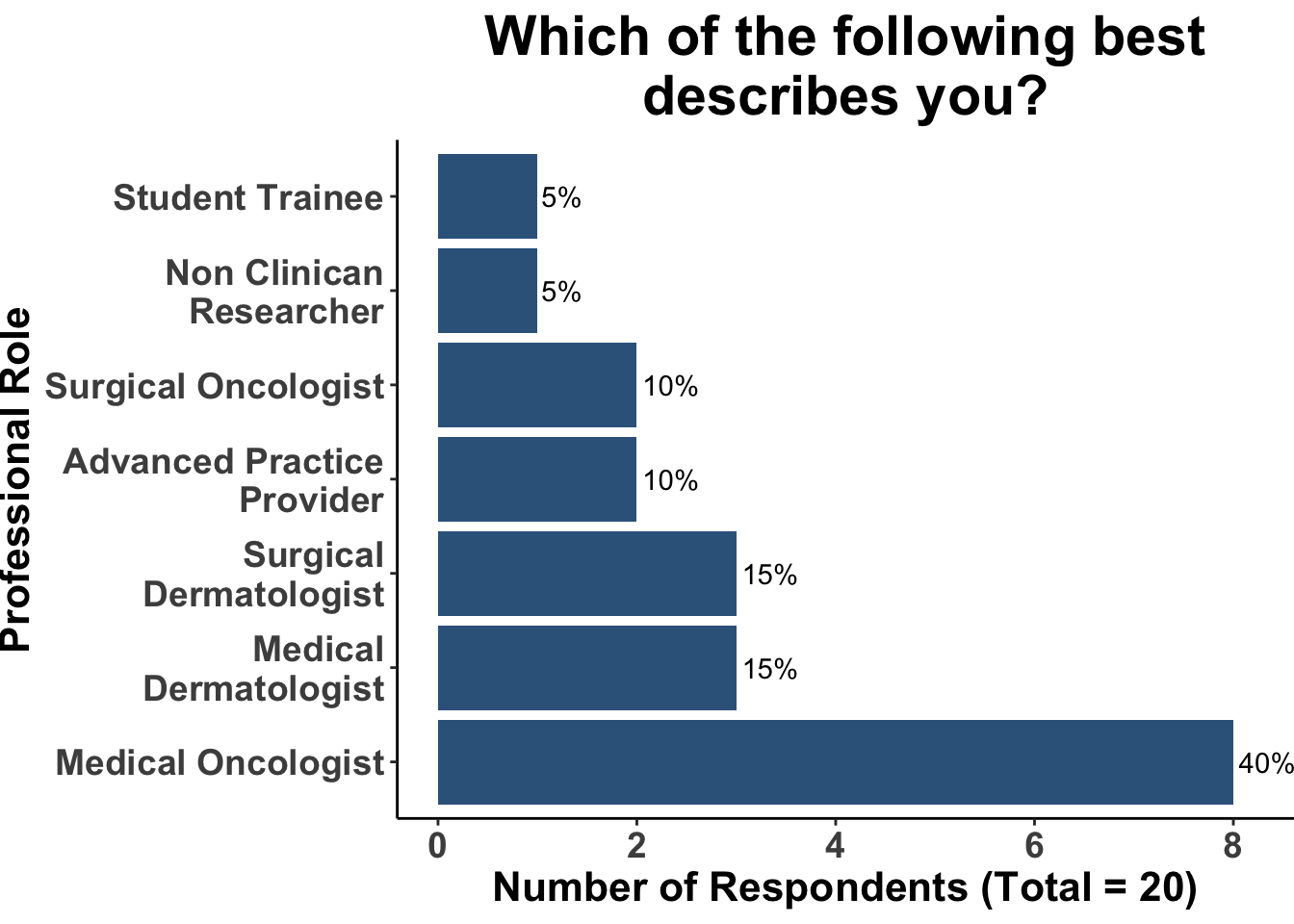
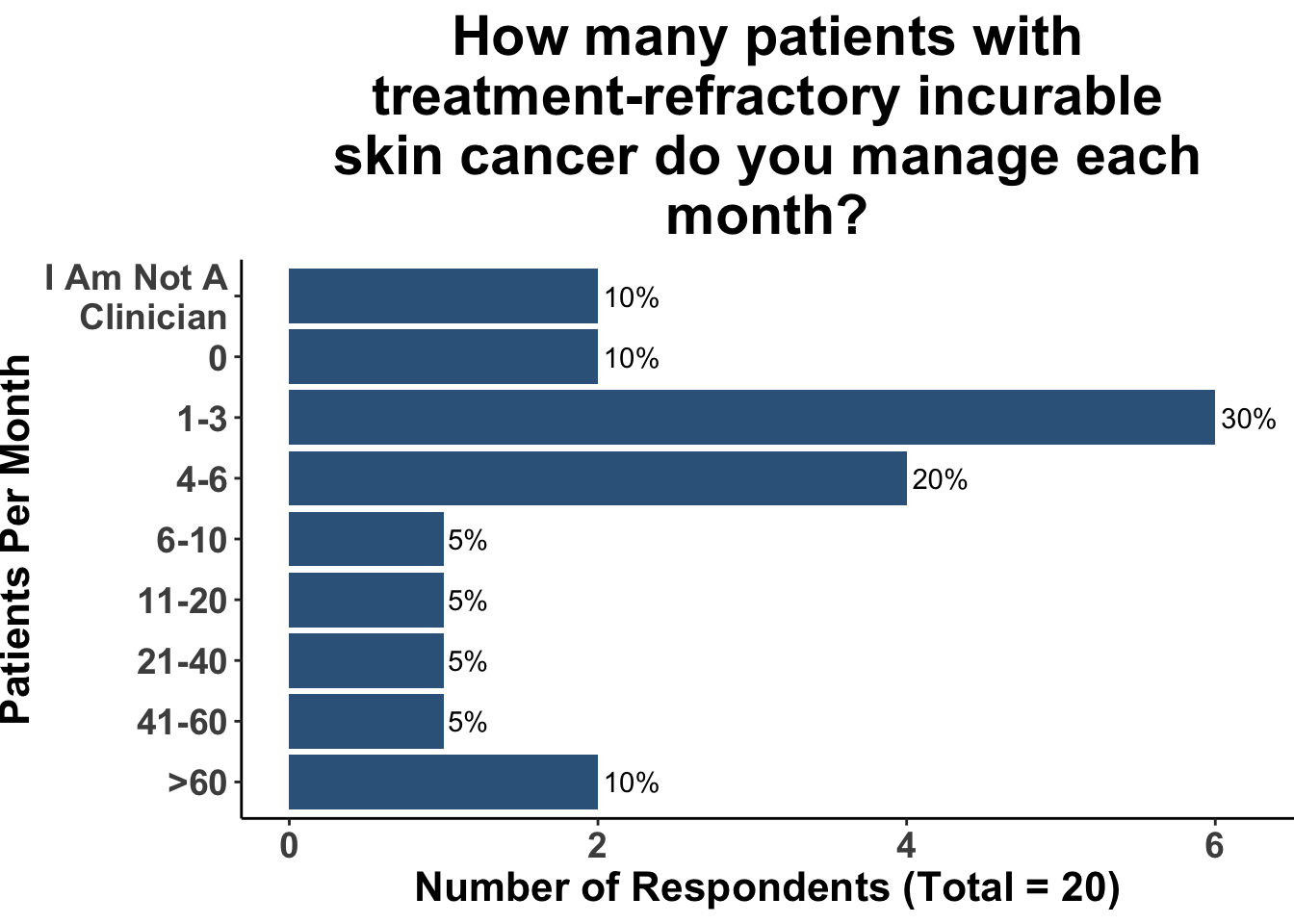
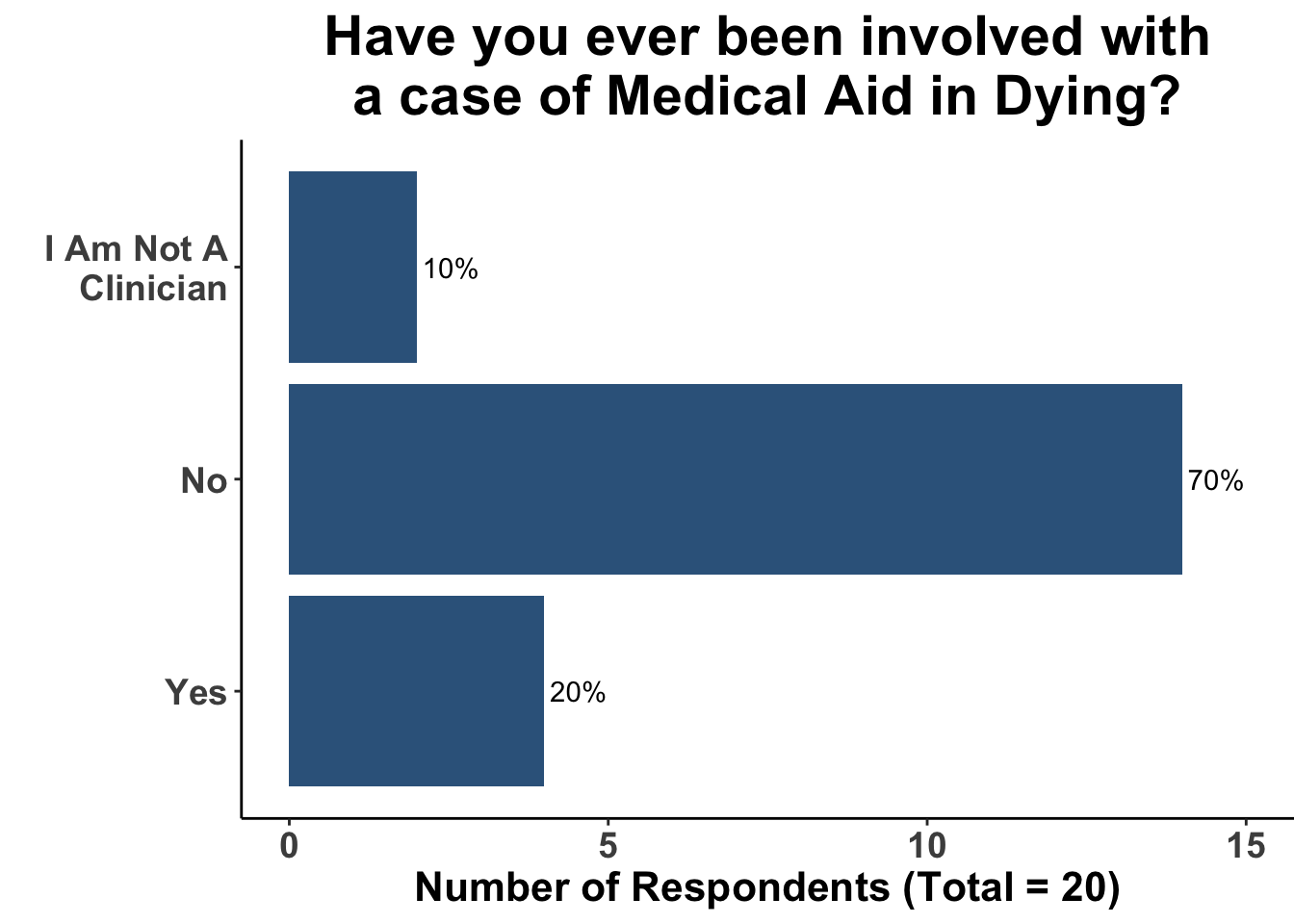
SoCO Journal Club participants including Medical Oncologists, Head and Neck Surgeons/Surgical Oncologists, Surgical Dermatologists, Medical Dermatologists, Advanced Practice Providers, and Student Trainees. This diversity reflects varying degrees of engagement with patients suffering from terminal cancers, as evidenced in Figures 2-3. However, given that MAiD is legally permitted in only a minority of U.S. states, only a select number of participants had personal experience with MAiD, as depicted in Figure 4.
Management of MAiD Cases
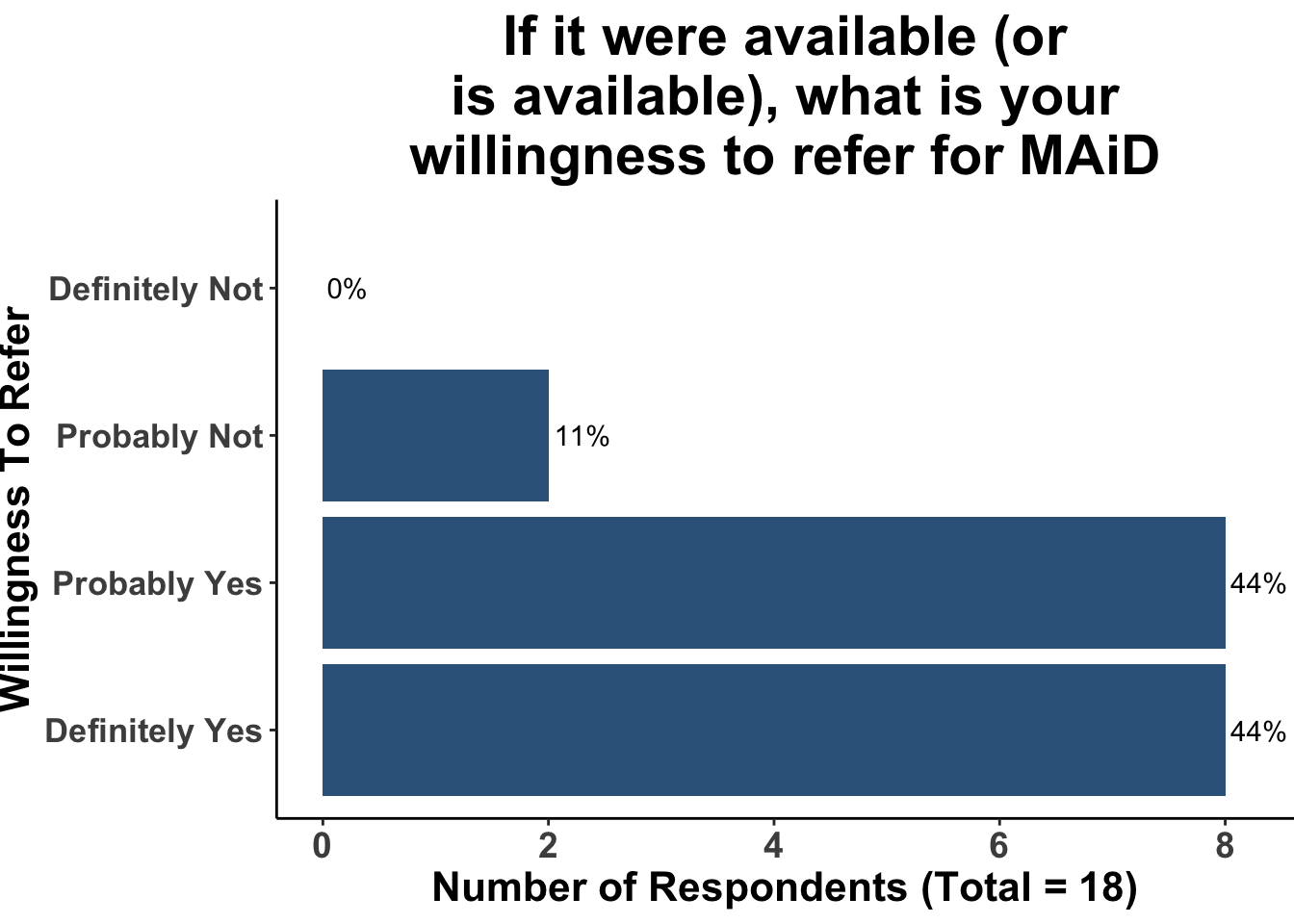
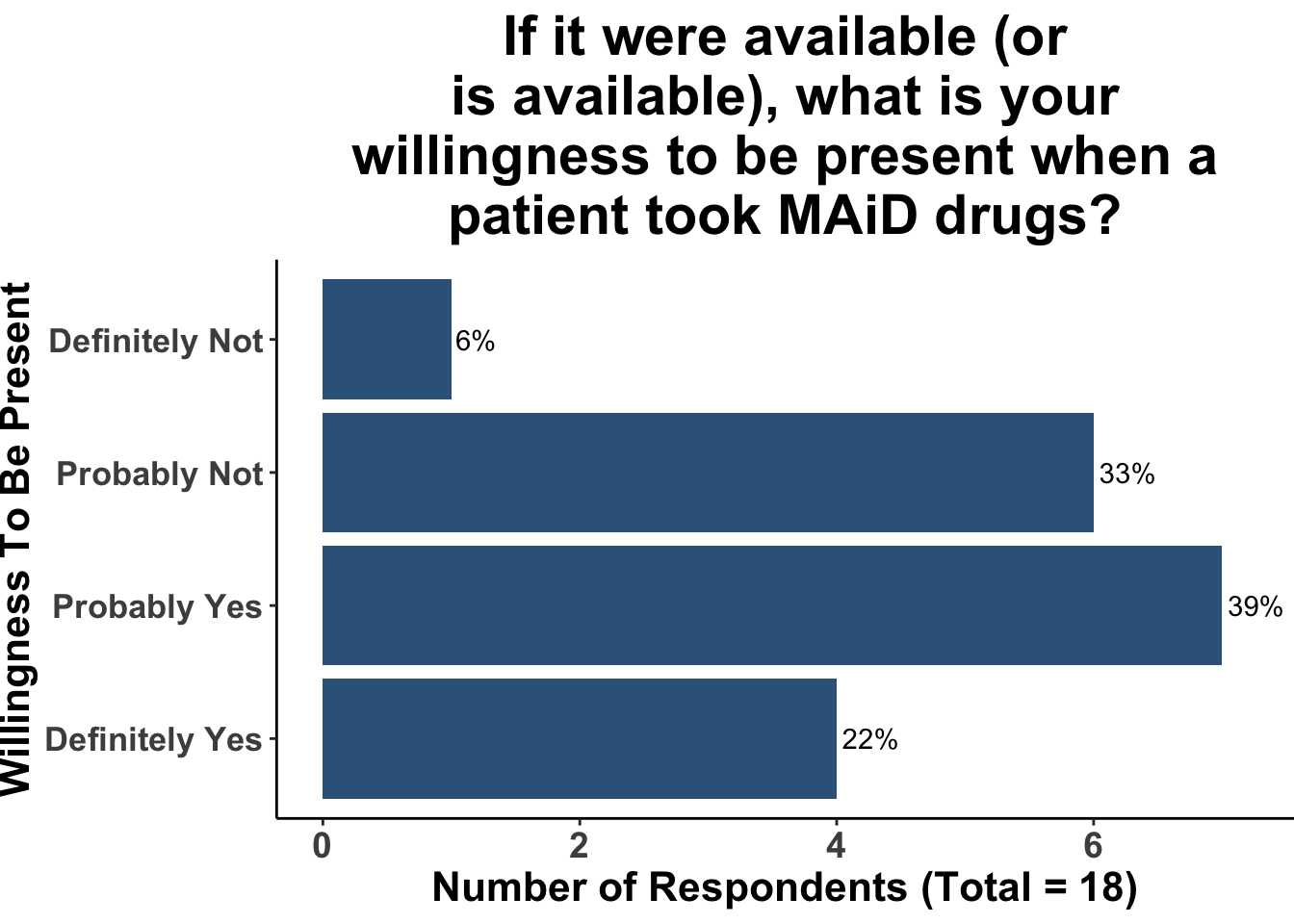
When asked about willingness to refer patients for MAiD, the vast majority of participants expressed conditional willingness, based on patient prognosis and quality of life considerations (Figure 5). In contrast, opinions on willingness to be presence during MAiD, were more split, highlighting the personal and ethical complexities of MAiD and potentially the differences in exposure to the practice among the participants (Figure 6).
Eligibility and Ethical Considerations
The survey responses revealed a diverse range of opinions on expanding the eligibility criteria for MAiD, reflecting the complex ethical landscape of this practice (Figure 7). A significant majority of respondents supported considering MAiD for adults in persistent vegetative states, acknowledging the irreversible nature of these conditions and the ethical imperative of respecting patient dignity in such circumstances. Similarly, a substantial proportion showed openness to including adults with late-stage dementia, recognizing the progressive and debilitating nature of the disease and the challenges in honoring the autonomy and prior wishes of these individuals. The discussion highlighted the importance of individuals creating advanced directives while they are fully capable, ensuring that, should they later lose the capacity to make or communicate decisions, their desires for MAiD are clearly documented and can be honored. The discussion also highlighted the ethical challenges that would accompany expanding MAiD to individuals who lacked capacity for decision making.
The perspective on adults with intractable chronic pain was more divided, with just over half of the respondents in favor. This viewpoint underscores the role of physical suffering in MAiD eligibility and the potential limits of palliative care in providing relief as well as defining what “intractable” means in this situation. In contrast, a smaller group of respondents considered MAiD for adults with intractable psychiatric conditions, raising critical questions about mental health, decision-making capacity, and the subjective nature of suffering.
In regards to extending MAiD to children with terminal conditions, nearly half of the respondents advocated for this consideration. This stance introduces a delicate debate about pediatric care, emphasizing the need to balance the child’s best interests with ethical considerations around maturity, decision-making capacity, and parental or guardian involvement.
Comparing the survey results from our SoCO Journal Club with those from the Colorado physicians study reveals some interesting points, albeit with limitations in drawing concrete conclusions. In our survey, 80% supported MAiD for adults in persistent vegetative states, compared to 68% in Colorado. For adults with intractable chronic pain, our support was slightly higher (55%) than Colorado’s (46.3%). In the context of intractable psychiatric conditions, our survey a higher level of support (30%) compared to Colorado (15.7%). Concerning late-stage dementia, our survey indicated 70% support, versus Colorado’s 48.6%. For children with terminal conditions, we observed a marginally higher inclination (45%) compared to Colorado’s physicians (41.1%).
It is important to note, however, that these comparisons are limited by differences in survey methodology and settings. Our survey’s context, participant composition, and possibly even regional medical and ethical cultures might differ significantly from those in Colorado, restricting the extent to which we can make direct inferences or draw conclusive comparisons between the two datasets.
Implications for Practice and Policy
Ultimately, the findings from Colorado14 and our SoCO Journal Club survey illustrate the need for nuanced, carefully crafted policies that balance respect for patient autonomy with the protection of vulnerable populations. As MAiD continues to evolve, ongoing dialogue among clinicians, ethicists, patients, and policymakers is essential. This conversation should be informed by interdisciplinary perspectives and committed to understanding the intricacies of end-of-life care, ensuring that MAiD remains a compassionate and ethically grounded practice.
As SoCO clinicians care for patients with advanced cutaneous malignancies, we are often called upon to help patients with decision-making around treatment options and end-of-life strategies. As such, a thorough understanding of MAiD and the logistics involved are important for all physicians who see advanced skin cancer patients. Physicians with a comprehensive understanding of this topic can help drive critical thinking during the development of legislation and policy adoption and compassionately assist patients at a difficult point during the course of their advanced cutaneous malignancy.
Materials and Methods
This Perspectives on the Science piece was published using Quarto®. The survey was conducted using REDCap®.15 The figures depicting the survey data were created using R (version 4.0.0) and the tidyverse suite of packages,16 including ggplot2.17 Interactive figures were made with ggplot2 and plotly18. The image on the “Perspectives on the Science” page was created by the authors (DMM) using the rosemary package.19 GPT-4, a language model developed by OpenAI, was employed in the drafting and editing of this manuscript. GPT-4 provided assistance in manuscript structuring, and generation of content, ensuring a comprehensive and cohesive presentation of the research and discussion points.20
Bibliography
Appendix
Citation
@article{miller2024,
author = {Miller, David M. and Brownell, Isaac and Tchekmedyian,
Vatche and Patel, Vishal A. and Kaufman, Howard L. and Emerick,
Kevin S},
publisher = {Society of Cutaneous Oncology},
title = {Perspectives on {Medical} {Aid} in {Dying:} {A}
{Multifaceted} {Ethical} {Discussion}},
journal = {Journal of Cutaneous Oncology},
volume = {2},
number = {1},
date = {2024-03-01},
url = {https://journalofcutaneousoncology.io/perspectives/vol_2_issue_1/medical_aid_in_dying/},
doi = {10.59449/joco.2024.03.01},
issn = {2837-1933},
langid = {en}
}