Evaluation of clinical characteristics and pre-biopsy impressions of primary Merkel cell carcinoma of the skin
Article and Authorship Details
Journal: Dermatology Online Journal (postprint). Accepted August 13, 2021. © The Regents of the University of California, Davis campus. Please see the publisher’s version on the Dermatolgoy Online Journal website
Authors: Farees Saqlain, BA1, Sophia Z. Shalhout, PhD1,2, Kayla Wright, BA2, and David Michael Miller, MD, PhD1,2,3
Affiliations:
1 Harvard Medical School, Boston, MA
2 Department of Medicine, Division of Hematology/Oncology, Massachusetts General Hospital, Boston, MA
3 Department of Dermatology, Massachusetts General Hospital, Boston, MA
Keywords: Merkel cell carcinoma, diagnosis, staging
Funding sources: This work was supported by Project Data Sphere, the American Skin Association, and ECOG-ACRIN.
Potential conflicts of interest: The authors declare no conflicts of interest.
Abbreviations:
BCC: Basal Cell Carcinoma
MCC: Merkel Cell Carcinoma
NMSC: Non-melanoma Skin Cancer
NOS: Not Otherwise Specified
NUB: Neoplasm of Uncertain Behavior/Neoplasm Not Otherwise Specified
SCC: Squamous Cell Carcinoma
UV: Ultraviolet Radiation
To the Editor:
Compounding its great propensity for metastasis and an increasing incidence, Merkel cell carcinoma (MCC) typically presents with primary cutaneous tumors that vary widely in appearance and are prone to misdiagnosis, even by experienced dermatologists [1,2]. Here we provide data on pre-biopsy clinical impressions of primary cutaneous MCC tumors from a cohort of 232 patients diagnosed with primary MCC between 2016 and 2019 available from the Mass General Brigham medical record [3]. Despite improved awareness in the last decade, in part due to successful immunotherapy development programs and the Merkel Cell Carcinoma Multi-Center Interest Group [4], we find that MCC continues to be rarely included in the clinical differential prior to biopsy. We discuss several observed trends in clinical diagnosis, and propose a subset of primary tumors that may be especially prone to escaping clinical suspicion as MCC.
This study was approved by the MGB IRB Protocol# 2019P002459. 59.5% of the cohort were male (n = 138/232), 78.0% (n = 181) were over 65 years old, and 96.6% (n = 224) were white. The majority of primary cutaneous tumors were located on the head, neck, or extremities (86.6%) (Table 1; Figure 1A). 61.7% of tumors were less than or equal to 2 cm in diameter on clinical exam (Table 1). 83% of cases (192/232) had at least one pre-biopsy clinical impression available within the clinician note or clinical history section of the pathology report (Table 1). The top three impressions were cyst (33.3%, or 64/192 cases), basal cell carcinoma (BCC; 31.8%), and squamous cell carcinoma (SCC; 19.8%) (Figure 1B). MCC was included in the differential in only 13 cases (6.8%), comparable to Heath et al.’s observed rate of 2 out of 106 (1.9%) in their 2008 review (Table 2) [5]. The majority of correctly diagnosed tumors were less than or equal to 2 cm in diameter on exam (11/12) and located on the head or neck (8/13). Correct diagnoses were primarily made by dermatologists (11/13 cases) practicing in either academic or community settings. In the 192 cases with pre-biopsy differentials, no primary care provider ever correctly suspected MCC, stressing the continued need to raise awareness of the disease in this essential provider group.
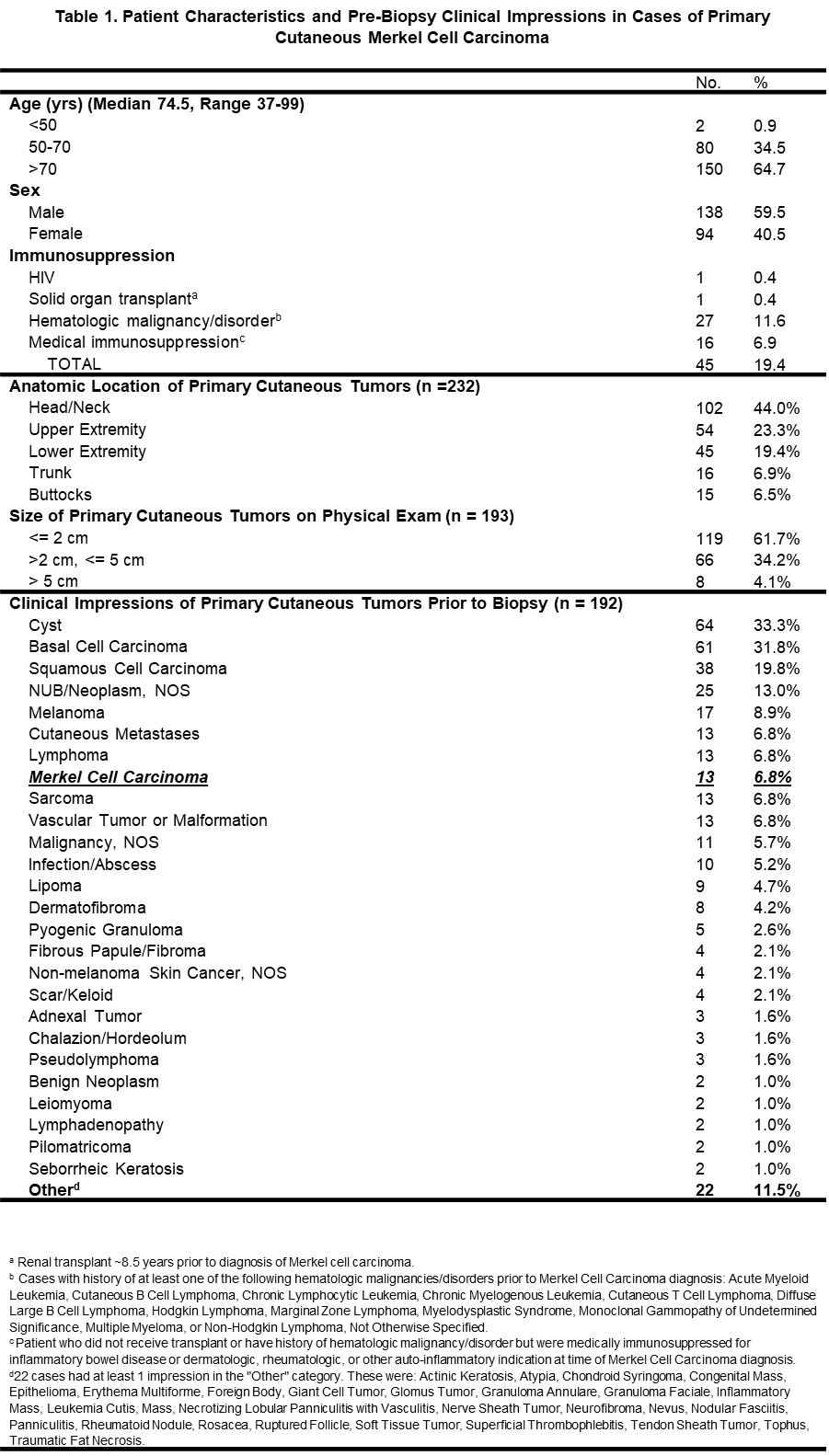
Table 1. Patient Characteristics and Pre-Biopsy Clinical Impressions in Cases of Primary Cutaneous Merkel Cell Carcinoma
Patient characteristics and distribution of anatomic location, tumor size on physical exam, and clinical impressions for a 5-year cohort of patients diagnosed with primary cutaneous Merkel Cell Carcinoma. NOS = Not Otherwise Specified.
 Figure 1A. Anatomic Distribution and Pre-Biopsy Clinical Impressions of Primary Merkel Cell Carcinoma Tumors
Figure 1A. Anatomic Distribution and Pre-Biopsy Clinical Impressions of Primary Merkel Cell Carcinoma Tumors
Anatomic distribution of primary cutaneous Merkel cell carcinoma tumors, restricted to cases for which pathology report was available to confirm location of primary tumor (n = 228). Lesions correctly suspected as MCC prior to biopsy are represented in red (n = 13/228).
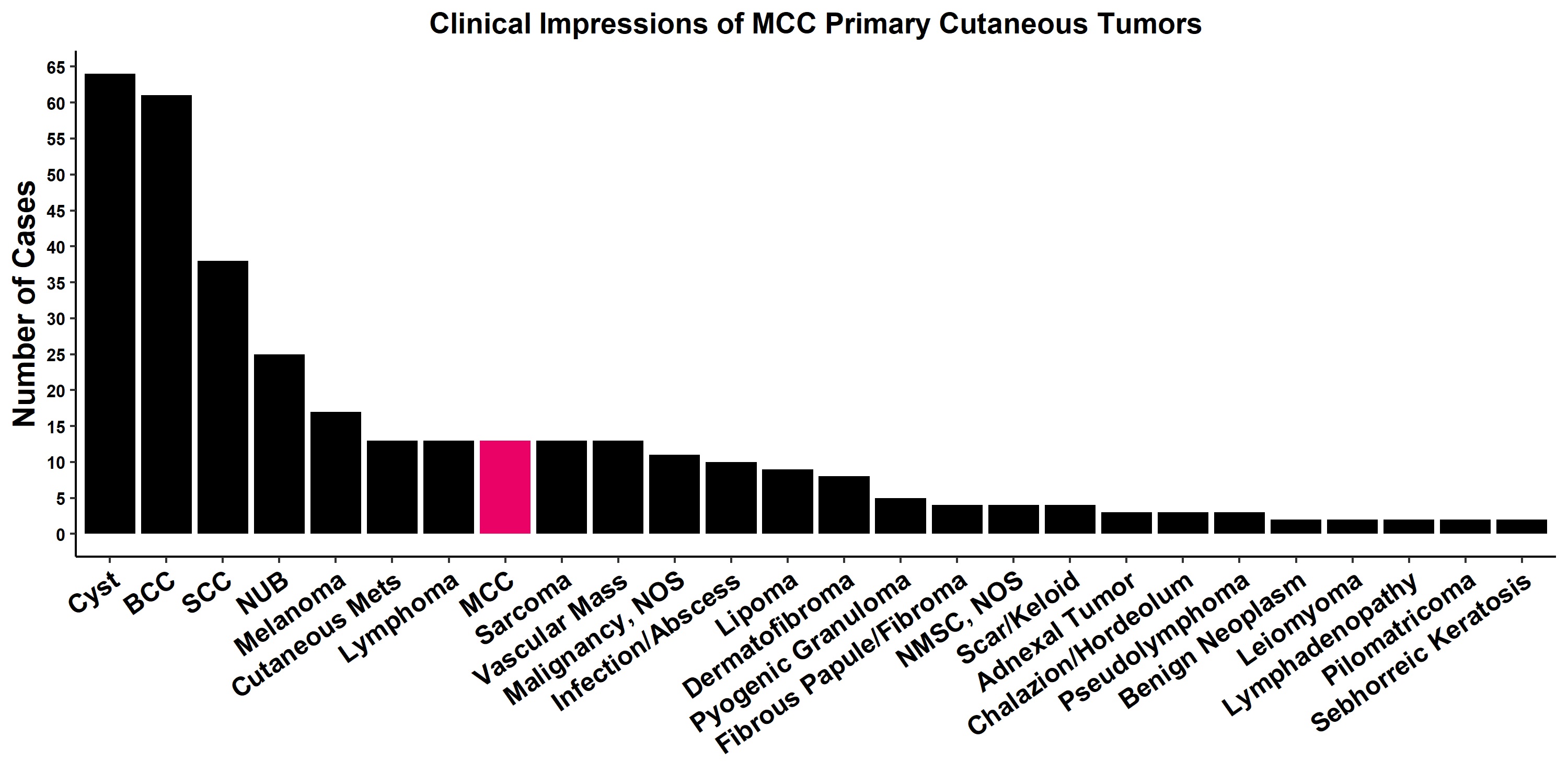 Figure 1B. Anatomic Distribution and Pre-Biopsy Clinical Impressions of Primary Merkel Cell Carcinoma Tumors
Figure 1B. Anatomic Distribution and Pre-Biopsy Clinical Impressions of Primary Merkel Cell Carcinoma Tumors
Histogram illustrating number of cases of primary cutaneous MCC in which the listed pre-biopsy clinical impressions were made (n = 192). BCC = Basal Cell Carcinoma, MCC = Merkel Cell Carcinoma, NOS = Not Otherwise Specified, NUB = Neoplasm of Uncertain Behavior/Neoplasm Not Otherwise Specified.
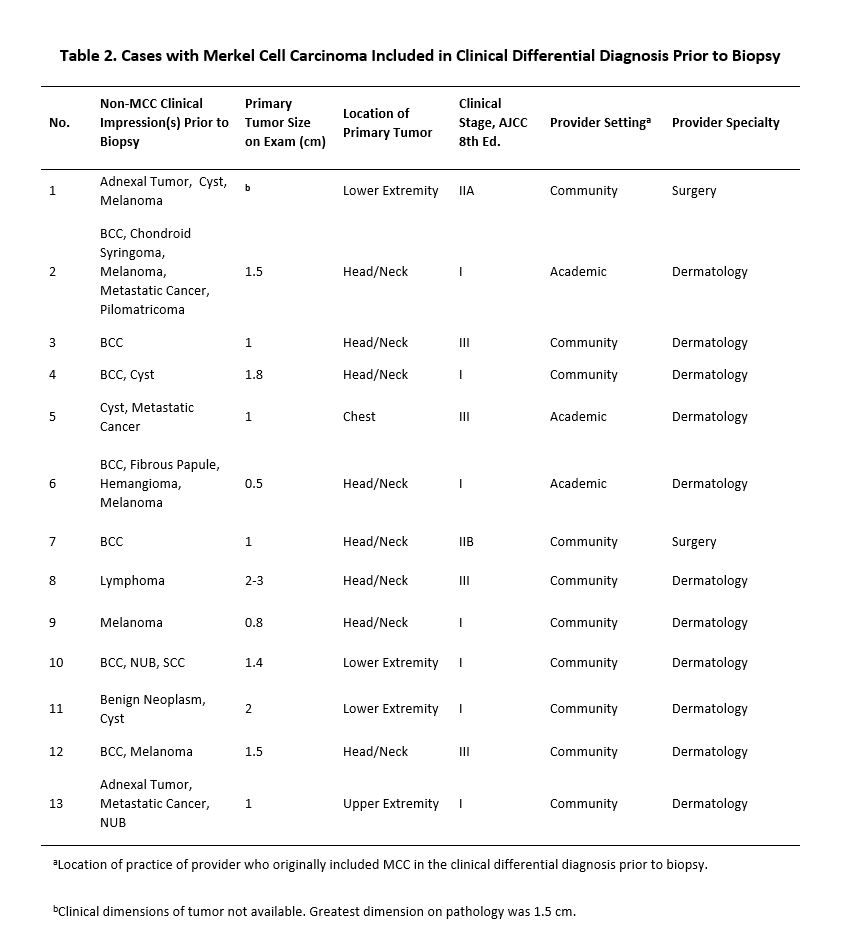
Table 2. Cases with Merkel Cell Carcinoma Included in Clinical Differential Diagnosis Prior to Biopsy
Non-MCC impressions, tumor features, staging, and provider setting in which diagnosis was made for cases in which Merkel cell carcinoma was correctly suspected prior to biopsy. BCC = Basal Cell Carcinoma, MCC = Merkel Cell Carcinoma, NUB = Neoplasm of Uncertain Behavior/Neoplasm Not Otherwise Specified, SCC = Squamous Cell Carcinoma
We highlight two suggestive trends from our retrospective review, acknowledging that any trend likely reflects a combination of phenotypic variability in MCC primary lesions as well as unaccounted biases in clinician diagnoses. First, only 1 out of 63 lesions over 2 cm in size with impressions available (1.6%) was correctly suspected as MCC, versus 11 of 108 tumors with diameters less than or equal to 2 cm (10.2%) (Table 2). Second, only 1 out of 38 cases with SCC on the differential (2.6%) also included MCC, a case where BCC was notably also on the differential (Table 2). In contrast, including the latter case, 7 out of 61 BCC-resembling lesions (11.5%) were correctly suspected as MCC. Together, these observations suggest that larger lesions or lesions conventionally “squamous cell” in appearance, likely with hyperkeratosis or scale, may be less likely to draw clinical suspicion for MCC. Due to the retrospective nature of this study, comprehensive data on clinical appearance of primary lesions at presentation was not available. While our ability to draw conclusions is consequently limited, and while confounders may exist, we suspect that our observations reflect clinician anchoring on a concept of primary MCC as a smooth, small or intermediately sized, erythematous papule on the head and neck in real-world practice. This is commensurate, for instance, with how the Skin Cancer Foundation describes the average Merkel Cell Carcinoma primary lesion on detection [6].
Interestingly, the proportion of SCC-resembling primary tumors, as evidenced by inclusion of SCC in the differential (38/192, or 19.8%), was similar to the reported frequency of tumors that display a “combined” histology in the literature. In 2018, Carter et al. found that <20% of MCC featured both neuroendocrine and other carcinomatous or sarcomatous, most often squamous, histology; strikingly, all were Merkel cell polyoma virus-negative [7]. Given that 92% of SCC-resembling tumors (35/38) were located on sun-exposed regions of the head, neck, and extremities, we hypothesize that the contrasting macroscopic phenotypes of “scale versus no scale” may be associated with the dichotomous pathogenesis of virus-negative/UV-driven MCC vs. virus-positive MCC, respectively. Our data on polyomavirus immunohistochemistry and seropositivity on this retrospective cohort is incomplete. The proposed association is therefore speculative and merits further inquiry with follow-up studies utilizing tissue profiling data. In any case, raising awareness specifically for this posited less frequent phenotype of primary tumors may improve clinical diagnosis rates of MCC by dermatologic and non-dermatologic providers.
References:
1. Harms KL, Healy MA, Nghiem P, et al. Analysis of Prognostic Factors from 9387 Merkel Cell Carcinoma Cases Forms the Basis for the New 8th Edition AJCC Staging System. Ann Surg Oncol. 2016;23:3564–71. [PMID: 27198511].
2. Paulson KG, Park SY, Vandeven NA, et al. Merkel cell carcinoma: Current US incidence and projected increases based on changing demographics. J Am Acad Dermatol. 2018;78:457-463.e2. [PMID: 29102486].
3. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. [PMID: 18929686].
4. MCC Multi-center Interest Group. n.d. https://merkelcell.org/about-us/mmig/ (accessed February 16, 2021).
5. Heath M, Jaimes N, Lemos B, et al. Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: the AEIOU features. J Am Acad Dermatol. 2008;58:375–81. 6. Merkel Cell Carcinoma Warning Signs. Skin Cancer Foundation. 2019.
https://www.skincancer.org/skin-cancer-information/merkel-cell-carcinoma/mcc-warning-signs/ (accessed June 28, 2021).
7. Carter MD, Gaston D, Huang W-Y, et al. Genetic profiles of different subsets of Merkel cell carcinoma show links between combined and pure MCPyV-negative tumors. Hum Pathol. 2018;71:117–25. [PMID: 29079179].