Heme-Derm - Principles at the Intersection of Blood and Skin
Overview & Learning Objectives
- The objective of this lecture is to provide an overview of salient intersections between
DermatologyandHematology
- We will use the following cases as guides throughout the lecture
- These are a fictional cases.
- The first case is loosely based off one that was presented at a Clinical-Pathologic Case Conference when I was a House Officer at Brigham and Women’s Hospital.
- I have changed several aspects of the case to de-identify it, though the medical principles of the case remain intact. Thus, any direct relations to an actual patient is purely co-incidental.
- I do want to give my former colleague Dr. Timothy Churchill an acknowledgement, since the original case was written up by him, and the overall structure of that case remains intact.
- Again, all of the identifers (age, gender and non-essential diagnoses) have been randomly altered to preserve anonymity.
Clinical Cases
Of note, words in blue contain both a hyperlink to additional information and “hover text” capabilities, allowing you to hover over for additional info
Case One
A 48-year-old female with Hypoxemic Respiratory Failure and Progressive Skin Lesions
Synopsis
A 48-year-old female with a history of Mycosis Fungoides (MF), for which she received a myeloablative allogeneic stem cell transplant (ASCT), which was complicated by graft-versus-host disease (GvHD), was admitted for evaluation of dyspnea and subsequently transferred to the medical intensive care unit (MICU) for hypoxemic respiratory failure.
The patient had been healthy until seven years prior to the current admission when she was diagnosed with tumor stage MF. The patient’s skin cancer progressed despite treatment with phototherapy plus oral bexarotene, romidepsin, doxorubicin, pralatrexate, and gemcitabine. Eleven months prior to this current admission, she underwent total skin electron beam therapy followed by myeloablative conditioning and then a matched, related-donor allogeneic stem cell transplantation. The ASCT conditioning regimen consisted of cyclophosphamide and total body irradiation. Tacrolimus and methotrexate were used for prophylaxis against GvHD. Four months post-ASCT, she developed new cutaneous plaques, and findings from a skin biopsy were consistent with recurrent Mycosis Fungoides. The patient’s tacrolimus was tapered and eventually discontinued, with gradual improvement of her MF lesions. However, over the subsequent months, with tapering of her immunosuppression, she developed eye and skin changes consistent with severe GvHD.
Four months prior to the relevant presentation, the patient was hospitalized for hypoxemia and hypotension. A CT of the chest showed bilateral ground glass opacities. A thorough microbiologic evaluation including bronchoalveolar lavage was unrevealing. Unfortunately, the bronchoscopy was complicated by pneumomediastinum with severe subcutaneous emphysema; thus, additional attempts at diagnosis of lung findings were deferred. The patient was empirically treated for pulmonary GvHD with 2 mg/kg of methylprednisolone, followed by a two-week course of etanercept. The patient’s hypoxemia did not improve, and she was subsequently treated with a course of alemtuzumab, which resulted in significant improvement in her pulmonary status. After a 32-day hospitalization, the patient was transferred to a skilled nursing facility on 4-8 liters per minute of oxygen by nasal cannula. During this admission, she was also started on isoniazid treatment for potential latent tuberculosis, given history of a positive PPD, and prophylactic voriconazole, in addition to her prophylactic trimethoprim-sulfamethoxazole and acyclovir.
The patient’s pulmonary symptoms were stable until one week prior to the current and relevant admission. The patient’s dyspnea subjectively worsened on 8-10 liters per minute of oxygen, so she was transferred to a tertiary care hospital for evaluation. On admission, she denied cough, fevers, or chills. Computed tomography angiography of the chest was performed and did not reveal any pulmonary emboli, but did show persistent bibasilar bronchiectasis with peribronchial thickening and consolidative opacities, unchanged from the most recent imaging six weeks previously, as well as interval development of numerous, diffuse sub-centimeter pulmonary nodules, in a predominantly vascular distribution. The patient was treated empirically for healthcare-associated pneumonia with vancomycin and cefepime. Over the next four days, her oxygen requirements steadily increased, and she eventually required high-flow nasal cannula with an oxygen concentration of 75%. Blood, urine, and sputum cultures, drawn prior to administration of antibiotics, were sterile. Given her worsening oxygenation, the patient was started on 2 mg/kg intravenous methylprednisolone and transferred to the MICU.
The patient’s medical history was notable for atrial fibrillation, a positive PPD, in addition to the previously described mycosis fungoides, myeloablative SCT, and GvHD. At the time of transfer, her medications included cefepime 2 grams every 8 hours, vancomycin 1 g every 12 hours, trimethoprim-sulfamethoxazole single strength once daily, valganciclovir 450 mg twice daily, voriconazole 200 mg twice daily, methylprednisolone 60 mg IV twice daily, metoprolol tartrate 25 mg every 6 hours, aspirin 81 mg daily, atorvastatin 10 mg daily, and SQ heparin for VTE prophylaxis. She remained on topical corticosteroids and calcineurin inhibitors for cutaneous and ocular graft-versus-host disease.
The patient denied any drug or environmental allergies. She was single, lived in the suburbs of a New England City, and did not have any children. Prior to the diagnosis of Mycosis Fungoides, she worked in education. She did not use tobacco products, alcohol, or recreational drugs. Her family history was negative for early cardiovascular disease, pulmonary disease, or hematologic malignancies.
On physical examination, the heart rate was 96 beats per minute, the blood pressure was 124/84 mmHg, and the respiratory rate was 20 breaths per minute with an oxygen saturation of 100%. Oxygen was delivered via high-flow nasal cannula at 60 liters per minute, with an oxygen concentration of 75%. The patient appeared somnolent but was easily arousable and responded to questions with short but appropriate answers. Sclerae were anicteric, and pupils were equal and reactive to light. Oral mucosa was moist, and there were no oropharyngeal lesions. Breath sounds were diminished with scattered crackles throughout the bilateral lung fields. Heart sounds were regular, with a single S1 and physiologic splitting of S2; there were no murmurs or gallops. The jugular venous pressure was estimated at 6 cm of water. The abdomen was soft and non-tender. Bowel sounds were normal. Her lower extremities were warm and trace edema. Skin examination was notable for diffuse sclerotic plaques with salt-and-pepper pigmentation over much of her body. A stage I decubitus ulcer was noted over the thoracic spine without drainage.
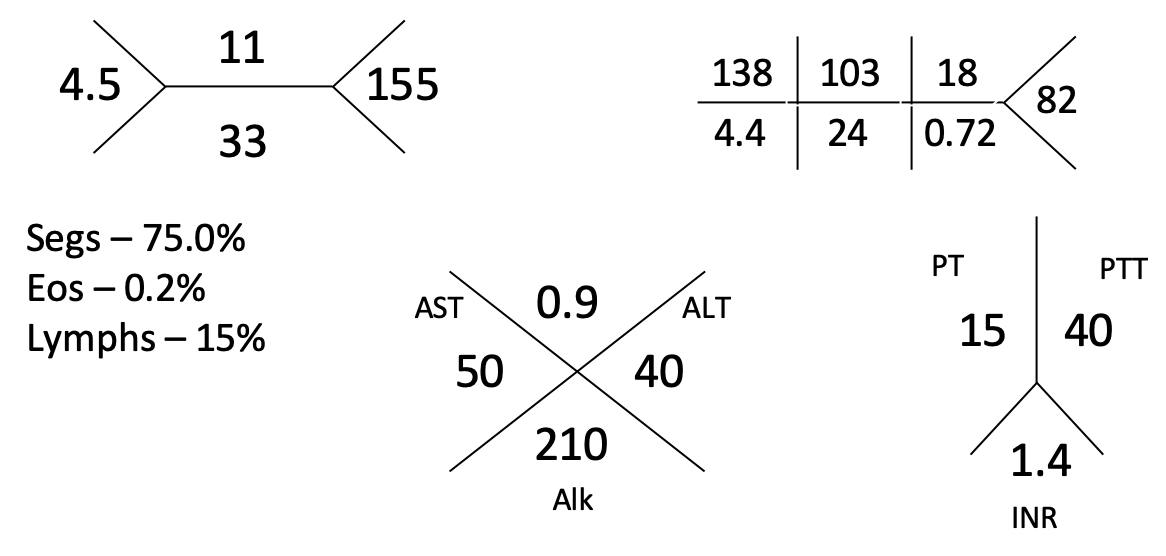
Laboratory analyses at the time of transfer revealed sodium 134 mmol/L, potassium 4.4 mmol/L, chloride 103 mmol/L, bicarbonate 24 mmol/L, blood urea nitrogen 12 mg/dL, creatinine 0.72 mg/dL, and glucose 82 mg/dL. The calcium was 8.8 mg/dL, magnesium 2.0 mg/dL, and phosphate 2.4 mg/dL. Liver function tests showed alanine aminotransferase 49 U/L, aspartate transaminase 55 /L, alkaline phosphatase 210 U/L, and total bilirubin 0.9 mg/dL. Arterial blood gas on 80% inspired oxygen showed a pH of 7.44, a partial pressure of carbon dioxide of 35 mmHg, and a partial pressure of oxygen of 288 mmHg. The white blood cell count was 6,500 per microliter, the hematocrit 26%, and the platelet count 280,000 per microliter, with a differential showing 81.0% polymorphonuclear neutrophils, 12% monocytes, 2% lymphocytes, and 0.2% eosinophils. The international normalized ratio was 1.4, and the partial thromboplastin time was 35.9 seconds.
N-terminal pro-brain natriuretic peptide was 110 pg/mL and troponin T was less than assay. A manual blood smear was examined and did not reveal any abnormal-appearing white blood cells or dysmorphic RBCs. Urinalysis had a specific gravity of 1.020, 1+ blood, and a pH of 7.6; leukocyte esterase and nitrites were negative. The urine sediment showed seven red blood cells, but no white blood cells, bacteria or crystals. Lactate dehydrogenase was 279 U/L. Serology for HIV was negative, and an interferon-gamma release assay was non-negative.
Echocardiography showed a normal-sized left ventricle, with an ejection fraction of 60% and evidence of impaired diastolic relaxation. The bilateral atria and right ventricle were normal in both size and function, and there was no significant valvular dysfunction. An agitated saline study was performed and was negative for intracardiac shunting. Galactomannan and Beta-D-glucan were negative. PCR for influenza, parainfluenza, RSV and adenovirus were negative.
Over the subsequent two weeks in the Medical Intensive Care Unit, the patient developed a progressively increasing oxygen requirement. Cefepime was subsequently changed to imipenem, and she was given alemtuzumab and methylprednisolone for a total of five days each, followed by a methylprednisolone taper. Repeat computed tomography of the chest revealed significant progression of the previously-noted numerous small lung nodules, which were present in all lobes and followed an angiocentric distribution.
Increased ground glass opacification of bilateral lung fields were also noted. A new, painful ecchymotic plaque, approximately 7 cm in diameter, was noted on the dorsum of her right foot. The plaque increased in size over the following 5 days, and a ~5 cm hemorrhagic bulla formed over the central portion of the plaque. A ~3 cm oval purpuric patch with a small hemorrhagic bulla was also noted on the left lateral shin.
Multiple, repeat blood cultures were negative. Fibrinogen was 599 mg/dL. Beta-D-glucan and galactomannan were repeated and were again found to be negative. Viral loads for EBV, CMV, and adenovirus were negative. Serologies for blastomyces and coccidiomycoses were negative, as were the serum antigen for Cryptococcus and the urine antigen for histoplasmosis. In the setting of worsening respiratory failure, elective intubation for bronchoscopy was proposed, but the patient ultimately declined this intervention, given the complications that she had suffered from a prior bronchoscopy and uncertainty regarding the likelihood extubation.
A diagnostic procedure was performed.
Case One Challenge Questions:
- What are your
top threediagnoses on the DDx in rank order of most likley to least likely?
- What would your
diagnostic procedureof choice have been?
Case Two
A 62-year-old-female with a Lower Extremity Rash
Synopsis
Case Two Challenge Questions:
- What are your
top threediagnoses on the DDx in rank order of most likley to least likely?
- What are your next steps in working up this patient?
Case Three: